Introduction
Under particular circumstances the body can lose excessive water loss from diarrhea or sweating especially this year when the humidex was high in many areas of North America, or excessive blood loss due to hemorrhage. Whenever these situations occur it can upset the fluid balance of the body, arterial blood pressure and the amount of filtrate produced in the kidney. Both these circumstances result in blood pressure (BP) drop. In this article we will discuss how the body reacts to these extraordinary conditions in its attempt to normalize the situation to establish physiological balance or as some refer to as Homeostasis.
Hormonal control/Osmotic sensing
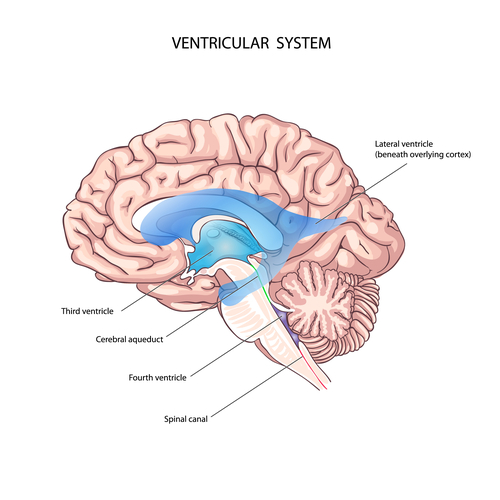
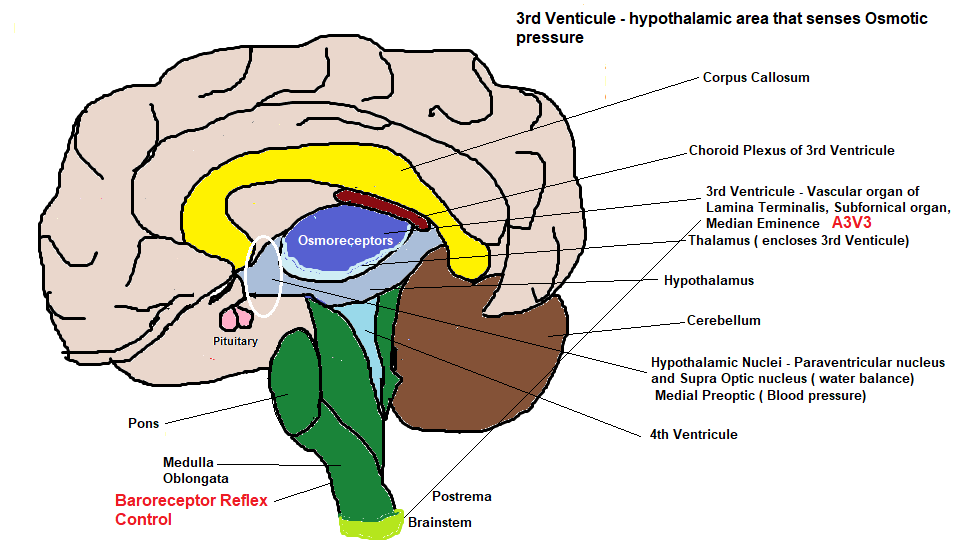
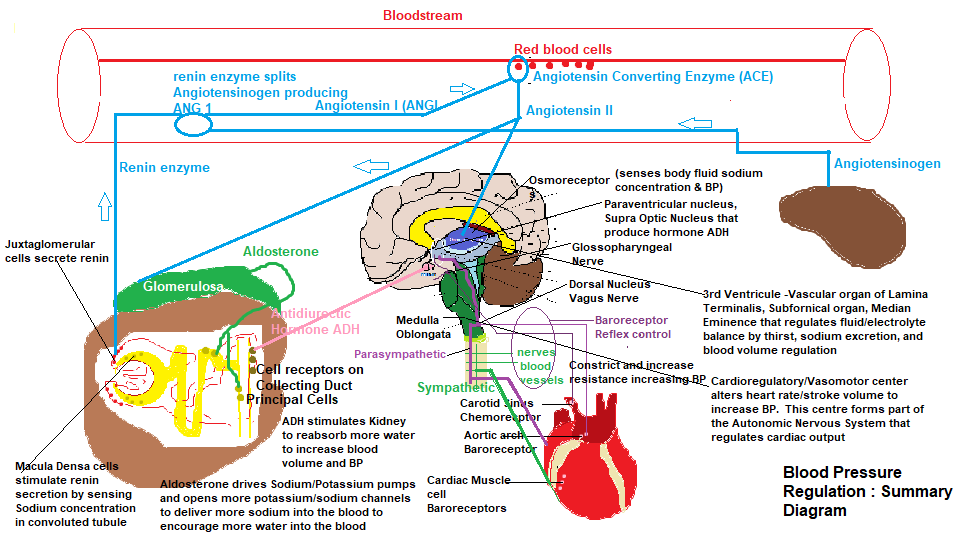
When fluid imbalance occurs, such as the conditions described above, osmotic pressure changes are detected by special cells called osmoreceptors that sense sodium content in the body’s fluids and osmotic pressure of the blood, that initiates the Supraoptic nucleus, which is a collection of magnocellular neurosecretory cells that initiate vasopressin(ADH hormone) production and transports it to the pituitary gland, that stores this hormone, via long dendritic neurons The third ventricle region of the brain shown in the diagram below is surrounded by 4 circumventricular organs that link to the central nervous system and peripheral blood using permeable capillaries (not connected to the blood brain barrier, providing an alternative route for hormone transport). The purpose of these sensory organs is the regulation of fluid and electrolyte balance controlling thirst, sodium excretion, blood volume regulation and ADH secretion. In effect this region known as AV3V sets up a positive feedback loop with the Angiotensin II hormone that stimulate receptors in the ‘Vascular organ of lamina Terminalis’. The other sensory organs within A3V3 includes the ‘Subfornical organ’ (involved in fluid balance and energy homeostasis), ‘Median eminence’ (responsible for regulatory hormone secretion), and the ‘Postrema’ The Postrema actually resides in the brain stem just below and behind the 4th ventricle and its made of ependymal cells which constitutes the thin neuroepithelial lining of the brains ventricular system (comprised of 4 interconnected cavities ( ventricles) where cerebrospinal fluid (CSF) is produced). CSF acts as a cushion to protect the brain, immunologically, and mechanically, ). The purpose of the Postrema is to control vomiting.
Low blood volume and low blood pressure sensing
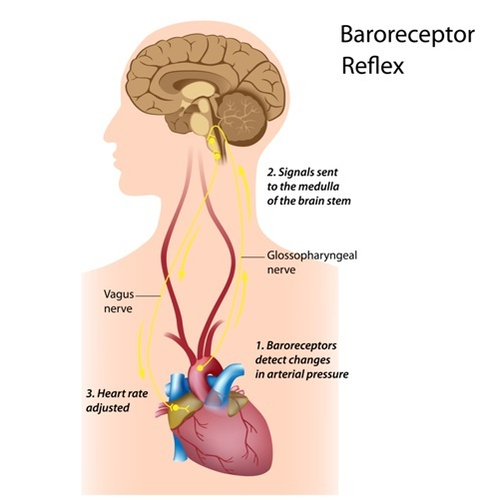
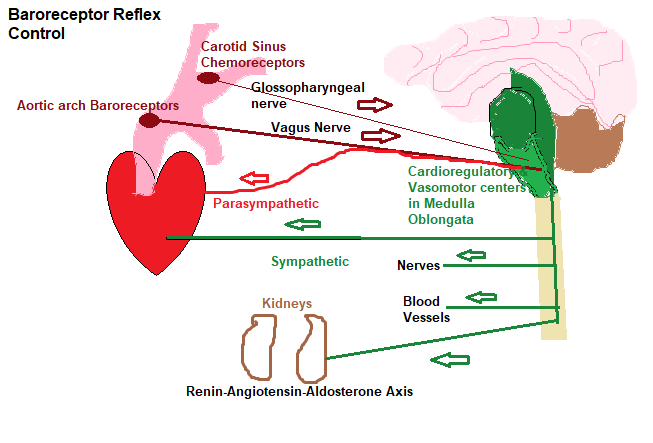
In the case of water loss due to excess sweating, the osmoreceptors trigger the Pituitary gland to secrete a hormone Antidiuretic (ADH), that is sent to the kidney, activating the collecting ducts to reabsorb more water, thus preventing excess water loss through the urine. There is a biological connection between the Supraoptic nucleus and the pituitary using nerve cells containing ADH just waiting to be secreted as described in the last paragraph. ADH secretion stimulates the cells lining the collection ducts in the kidney, to reabsorb more water, and transport it to the bloodstream, thus increasing blood volume and blood pressure to normal levels, but if the solute becomes too low, then ADH discontinues allowing excess water to be eliminated. Blood volume is actually a measure of the total blood concentration, including all solutes which is referred to as Osmolarity measured in Osmoles/litre. The normal range is between 280-300 osmoles/litre, and anything below ( too dilute) or above (too salty) activates the ADH trigger from the pituitary gland. Baroreceptors (pressure sensors) located in the Aortic arch ( If you have read the article on ‘unblocking the blood pipes’ the Aorta distributes blood from the left ventricle of the heart to the rest of the body), and the carotid sinuses that reside in the carotid arteries adjacent to the aorta , sense low blood volume. The carotid sinus sense receptors are known as ‘Chemoreceptors’ that ‘surveille’ the blood for diminished blood flow, causing a decrease in oxygen, excess accumulation of carbon dioxide and hydrogen ions, as well as Angiotensin II ( to be discussed later ). This blood pressure sensing system, using the baroreceptors and the chemoreceptors , transmit signals to the Cardioregulatory/vasomotor center located in the medulla oblongata as shown in the diagram ‘ Baroreceptor reflex control’ diagram.
The purpose of Aldosterone and blood pressure
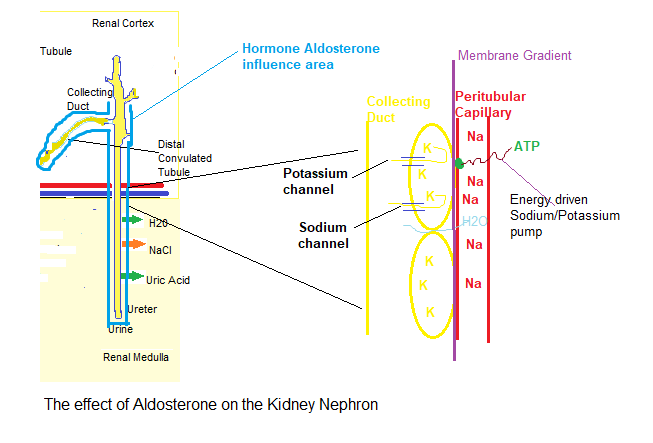
Another hormone, Aldosterone, that is involved with blood volume, is secreted by the Adrenal gland is also triggered by angiotensin II ( soon to be discussed..lol), but what does aldosterone do?……the simple answer is it raises blood pressure…..how ?. We discussed the HPA (Hypothalamus-Pituitary Axis) stress axis in a previous article, and I have recreated the diagram below. The glomerulosa, which is part of the adrenal cortex, is responsible for manufacturing Aldosterone on demand, from cholesterol that resides in its cells. This low blood pressure demand is triggered by the presence of Angiotensin II (wait.. I’m getting to it..lol) or the rise of Potassium ions in the bloodstream.

Once aldosterone reaches the kidney, it influences the principal cells that line the distal convoluted tubule and the collecting duct as shown in the diagram below: The principal cells contain a good amount of Potassium (K+), while the blood flowing in the peritubular capillaries contain a good amount of Sodium (Na+). Although Sodium is principally responsible for osmotic * water flow, other salts within the blood such as Chloride (Cl-), Potassium (K+) and Magnesium (MG2+) are also regulated during this process. The cells need to maintain the membrane gradient between the principal cells and the capillary blood, so there are many sodium/potassium pumps** in the cellular membrane that transport potassium into the cell and sodium out, into the blood. Aldosterone basically drives the sodium/potassium pumps harder to get more potassium into the cell and more sodium into the blood. Secondly it installs potassium channels into the cell, causing the potassium in the cell to flow into the collecting duct, thus encouraging the pump to move more potassium into the cell from the blood, so consequently the blood loses potassium. Thirdly it installs sodium channels onto the cellular membrane which encourage sodium to be pumped from the collecting duct into the cell and as a consequence, it gets pumped into the blood, so more sodium ends up in the blood. From an osmotic perspective water always follows a salt, sodium in this case, so water from the collecting duct will follow the sodium into the cell and then into the blood increasing blood volume (stroke volume) and blood pressure.
*An example of osmosis can be shown when pure water is placed on one side of a semi-permeable membrane, and a solution of sodium chloride on the other. Water passes through the cell membrane easily, but the sodium and chloride ions pass only with difficulty, displacing the water molecules. As this continues a pressure (osmotic pressure) difference is established that cause the sodium chloride to stop all together.
**The Na+-K+ pumps are also important to regulate cell volume, and without these pumps the cell would expand to a point of destruction. Within the cell, there are component proteins and other organic molecules that are ‘imprisoned’ in the cell, and being negatively charged, they attract large amounts of potassium.sodium and other positive ions. Furthermore, they cause osmosis to occur allowing water to flow into the cell. The pump actively transports 3 Sodium (Na+) ions out of the cell, for every 2 Potassium (K+) ions into the cell. Once the sodium ions are outside they tend to stay there, initiating osmosis out of the cell as well, and this surveillance to control cell volume is constantly active. Interestingly, by pumping 3 sodium ions to the exterior, and 2 potassium ions to the interior of the cell, creates a positive potential outside, and a negative potential inside the cell, creating an electrical potential across the cell membrane which is used to transmit nerve and muscle signals.
The Renin-angiotensin-aldosterone axis and the Juxtaglomerular Apparatus
As discussed in the last section the baroreceptor reflex control, as shown in the associative diagram, affects both branches of the autonomic nervous system (ANS) that have opposing effects on blood pressure. The sympathetic branch (Fight or flight), as you would expect, elevates total peripheral resistance ( blood vessel vasoconstriction ) and cardiac output, increasing contractility of the heart, and heart rate, increasing blood pressure. The Parasympathetic branch (rest and digest) has the opposite effect lowering blood pressure. By coupling sympathetic and parasympathetic activation, blood pressure is maintained at normal levels. So the baroreceptor reflex provides homeostatic balance, maintaining constant levels of normal blood pressure just as in a car, by using the gas and brake pedals. However, this system is triggered, as a rapid response during times of exercise for example, but for normal day to day activity a slower reacting system is activated called the Renin-angiotensin-aldosterone axis. So how does this work ?. It all starts in the liver which we will discuss in the next section.. If you have read the previous article you will remember the afferent and efferent arteriole that delivers blood to the glomerulus (Bowman’s capsule) in the kidney. Within these arterioles, are smooth muscle cells called ‘Juxtaglomerular’ cells that synthesize, store and secrete an enzyme called Renin which is triggered by stretch receptors built into the vascular wall, that sense low blood pressure. Low sodium concentration, another characteristic of blood imbalance, is also sensed by ‘Macula Densa’ cells located in the distal convoluted tubule, that also stimulates renin secretion by sensing a decrease in sodium concentration in tubular fluid. So, Juxtaglomerular cells and Macula densa cells both sense blood pressure, triggering renin secretion, but the third trigger as explained above are the sympathetic nerve cells. The Juxtaglomerular cells receive prostaglandin messenger proteins (Prostaglandins are hormone like messengers used for local cell to cell communication, and if you have read the article on omega 3 fatty acids you may recall that these are used to synthesize Prostaglandins) from the macula densa cells. The Juxtaglomerular cells also contain beta adrenergic receptors that are sensitive to epinephrine/norepinephrine released by sympathetic nerve cells.
The Juxtaglomerular apparatus
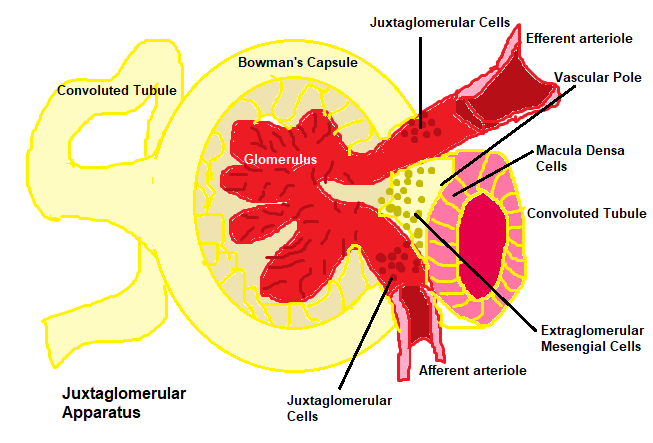
The Juxtaglomerular apparatus defines a cellular complex that include Juxtaglomerular and Macula densa cells, as well as another cellular complex called ‘Extraglomerular Mesangial cells’. These cells are located at the ‘vascular pole’ which is the junction where the afferent and efferent arterioles enter/exit the glomerulus of the kidney as shown in the diagram above. Another smooth muscle like cell, the Extraglomerular Mesangial cell is a ‘housekeeper’ whose primary function is to remove trapped residues and compacted protein fragments from the basement membrane of the glomerulus, keeping the filter free of debris. During early fetal development, these cells are involved in the formation of the convoluted blood capillaries allowing efficient diffusion to occur later, allowing the debris to be discarded through the endothelial cells of the blood vessels. These cells are a type of ‘Pericyte’, that are contractile cells, that wrap around the endothelial cells as they do in the brain to maintain blood brain barrier permeability, regulating capillary blood flow and the clearance of phagocytosis of cellular debris.
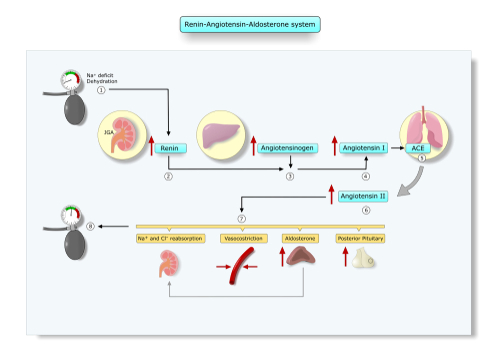
The Renin-angiotensin-aldosterone axis (RAAA) proper
As we stated earlier, it all starts in the liver where an RAAA precursor serum globulin protein called ‘Angiotensinogen’ is produced, and released into the bloodstream, where it floats around dormant until low blood pressure (Hypotension) is picked up by, either one of the 3 sensing systems, the Juxtaglomerular cells, macula densa cells or the sympathetic nerve cells which trigger the Juxtaglomerular cells to secrete the Renin enzyme into the bloodstream. Once there, it splits the protein angiotensinogen into a decapeptide ( 10 amino acid chain) called Angiotensin 1, which is converted by an Angiotensin converting enzyme (ACE), that resides in epithelial cells , the blood cells, lung, kidney and the brain to produce Angiotensin II. Recent research has identified the existence of an independent cardiac renin-angiotensin system (RAS), where the components of RAS necessary for Angiotensin II synthesis are present in the heart, so Renin, angiotensinogen (AGT), ACE and ANG II receptors exist in the myocardium. Furthermore, although renin and AGT concentrations are 1-4% of those in plasma, the cardiac interstitial fluid concentrations of ANG I & II are over 100 fold those of plasma. Since we are trying to elevate blood pressure angiotensin II triggers the following actions : .
- Systemic constriction of smooth muscle blood cells throughout the body increasing resistance and thus increasing blood pressure
- Stimulates the secretion of hormone Aldosterone from the adrenal gland whose target is the kidney.
Summary and conclusions
The diagram below summarises the various systems within the body, that senses low blood pressure(BP), from the loss of fluids due to diarrhea, or an excessive loss of blood volume, due to hemorrhage, which is rapidly stabilized by the autonomic nervous system, to the long term homeostatic Renin-Angiotensin-Aldosterone system (RAAS).
Blood pressure lowering drugs
Conventional medicine, when high blood pressure is diagnosed will prescribe a ‘quick fix’ solution by way of a blood pressure lowering drug. The pharmaceutical industry have developed many , which include ‘Diuretics’ of which there are 10 options, some cause excess potassium to be expelled from the body through urine, but some are potassium sparing. These drugs cause a multiplicity of side effects :
- Mineral imbalance, high uric acid and high urea levels, high blood sugar
- Low blood platelet count
- Muscle cramps, dizziness, hand tremor, dehydration, low blood pressure
- Kidney failure, vomiting, brain disease, abdominal pain, arthritic pain, chest pain
- Hyperventilation, diarrhea, impotence
- Coughing blood, severe or watery diarrhea, anemia
Alternatively Beta-blockers are prescribed, which can cause dangerously high blood pressure, upper respiratory infection, diarrhea, irregular heart beat, insomnia, edema, angina, and vomiting. Another BP medication are ACE inhibitors, that cause fatigue, dizziness, nausea, abnormal renal function. Other BP medications include Angiotensin II receptor blockers, Calcium channel blockers, Alpha blockers etc. The full list and their side effects can be found on rxlist.com : https://www.rxlist.com/high_blood_pressure_hypertension_medications/drugs-condition.htm
Looking at the summary diagram above I believe you can see that diuretic drugs interfere with water and salt (NAcl) reabsorption by lowering it, allowing more to be excreted through the urine. The RAAS mechanism is obstructed by ACE inhibitors and Angiotensin II receptor blockers, while calcium channel blockers slow the movement of calcium into the cells of the heart. Alpha blockers dilate blood vessels for example. Some drug candidates are prescribed more than one of these drugs, totally crippling the very processes that the body needs to adapt to changing conditions and circumstances that the host is involved with…..what happens if someone taking these chemicals wants to do exercise ??…how is the body supposed to increase BP to deliver more blood to the muscles, without that person experiencing angina, kidney failure, vomiting, hyperventilating or God knows what else, or they may begin to haemorrhage. These drugs put you potentially in harm’s way….don’t take my word for it just study the blood pressure regulation diagram above and ask yourself..would I take the risk ?…even Beta blockers actually can cause dangerously high blood pressure according to the RXlist site.
Possible causes of High blood pressure
We can consider the systemic blood system as a closed loop system that is under pressure, needed to ensure blood is pumped to every part of the body. Blood is crucial to distribute body heat, transportation of essential nutrients, respiratory gases, hormones, and to carry waste products out of the body. As you can appreciate from the diagram the body has many safeguards and feedback systems to maintain regulatory control of blood pressure. Blood pressure changes constantly in harmony with environmental stimulus, and the activity of the host, and the body intelligently adapts to these constant changes to maintain body balance and circulatory integrity. To accurately measure blood pressure it must be done over a 24 to 48 hour period using a device strapped to the arm ( called a Holter blood pressure device) that measures BP every 15 minutes or so. If this monitoring displays an almost constant high BP over a 1-2 day period than it is quite likely there is a physiological problem, with one or other of the 3 stressors that Dr B is always talking about, physical, chemical or emotional. Physical stress can occur due to a failure of an organ or structural damage to the ‘blood pipes’. More often than not, it is epithelial damage to the linings of the body’s tissues somewhere in the body, creating an inflammatory response. Chemical stress can be caused by a toxic nutrient deficient lifestyle such as eating man made food. Emotional stress could be caused by your own circumstances that you may be experiencing including a job related stress, divorce, loss of a close friend or parent, and/or financial worries etc.
To visit a conventional physician and accept a prescription for a BP lowering drug based on one BP reading is not only foolish, but it is harmful to the body, because these drugs, as I have explained above, work against your own internal body processes. Unless an organ has crashed or you are hemorrhaging , then the average physician cannot help you, because he/she does not know your lifestyle choices, nor are they interested. Their remit is to simply offer you a poisonous drug to lower your blood pressure no matter what the cause is. You have to empower yourself to fix the problem and allow the body to return to its default state of self healing and self regulating..and get on with your life healthy and happy.
Recent research
Angiotensin III & IV
We now now that the brain contains angiotensinogen, being 30% that found in the liver, and that the mRNA to produce it, resides in the astrocytes ( glial cell associated with the central nervous system). Furthermore Wright & Harding in their study “Angiotensin receptor subtype mediated physiologies and behaviors:New discoveries and clinical targets” published in 2007 confirms that not only does the brain contain all of the components to produce Angiotensin II but Angiotensin IV receptor also exists in the brain, implicated in cognitive processing, cerebral protection, local blood flow, stress, anxiety/depression, and renal tubular absorption which Angiotensin II has an inhibitory influence on, but a facilitatory role by Angiotensin IV. Even Gasparo et al ( 2000) & Speth et al ( 2004) suggested the existence of Angiotensin III ( converted by Angiotensin II using Glutamyl Aminopeptidase enzyme), that, alongside Angiotensin II, participates in the classical effects on body fluids and electrolyte homeostasis. To date the RAS in the brain has been well studied confirming its role in regulating central blood pressure by stimulating sympathetic nerve activity. There is even ACE2 that exists in the brain which opposes the effects of Angiotensin II, as well as Angiotensin II to angiotensin III conversion that occurs in the kidney. The study mentioned earlier by Wright & Harding also hypothesised that Captopril ( an ACE inhibitor drug) induced a sense of well being, less sexual dysfunction and an improved mental acuity at work as described from a 1986 study by Croog et al using 626 mild to moderate hypertensive patients. Well, all I can say is, that, patients must have overlooked the other side effects that include itching, chest pain, palpitations, fast heart rate, cardiac arrest, dizziness, coordination problems, confusion, depression, insomnia, swelling skin, sun sensitivity, acute renal failure, kidney impairment, impotence, abdominal pain, constipation, diarrhea, drowsiness, fatigue, loss of taste and appetite, nausea, vomiting, dry mouth, sores inside the mouth and lips, numbness in the hands and feet, HIGH BLOOD PRESSURE, enlarged man breasts, stroke, and the list goes on…and on..
Local RAS & the kallikrein–kinin system (KKS)
So, it appears that, apart from the classic circulating RAAS system, ‘local RAS’ systems exist, as confirmed from the previous paragraph. It is also suggested that there exists a local RAS system in the heart, and possibly the kidney itself, as described in the study performed in 2014 by De Mello and Frohlich entitled ‘Clinical perspectives and fundamental aspects of local cardiovascular and renal renin angiotensin systems’. Although it would appear that these local RAS systems function independently to the classic circulating RAAS. There must be some overlapping functionality between the systemic RAAS and the local RAS systems, but to date it remains undocumented. Finally, one more point, when tissue injury occurs, a plasma hormonal system is initiated, called the kallikrein–kinin system (KKS), which are blood proteins found in the pancreas, kidney, heart and adrenal gland, that cause vasodilation and decrease blood pressure. Research conducted in the 30’s identified a hypotensive substance produced in the pancreas that was named Kallikrein. Ten years later, another hypotensive substance was discovered, that was named Bradykinin, which eventually paved the way in developing the first antihypertensive drug Captopril (as discussed in the previous paragraph). When BP drops too low, the RAAS system triggers, inhibiting the Kallikrein-Kinin system, which is why the ACE inhibitor class of drug was developed, to cripple the RAAS mechanism promoting bradykinins to lower BP. Having said that, the research is non exhaustive on the KKS, and in some instances the KKS and RAAS exert common actions, as well as the recognized antagonistic relationship. We have to stay ‘tuned’ to future research to discover how the body uses circulating RAAS and the individual local RAS and their interfunctionalities, and how they affect KKS.
Check out other Articles in this series:
Nutrients in Food and their bodily purpose I (Phenols)
Nutrients in Food and their bodily purpose II (Lignans, Triterpenes, Phytosterols, Carotenoids & Fats)
Nutrients in Food and their bodily purpose III (Phenolic acids, sulphur, sulphides,sulphoxides )
Nutrients in Food and their bodily purpose IV (Glucosinolates, Sulforaphane, Indole-3-Carbinol)
Nutrients in Food and their bodily purpose V (Lipid distribution, absorbed fats, Criciferous Veg)
Nutrients in Food and their bodily purpose VI (Nutrients required for Liver Detox)
Nutrients in Food and their bodily purpose VII (Seeds & the Omega Fatty Acids)
Nutrients in Food and their bodily purpose VIII (Nutrients required for cellular energy production)
Nutrients in Food and their bodily purpose IX (Water I Properties and Body fluids)
Nutrients in Food and their bodily purpose X (Water II Cellular Hydration)
Nutrients in Food and their bodily purpose XI (Water III Fluid filtration, reabsorption, excretion)
Nutrients in Food and their bodily purpose XIII (Water V Body Fluid Dysfunction
Nutrients in Food and their bodily purpose XIV (Dental Nutrients)
Nutrients in Food and their bodily purpose XV (Nutrients involved in Methylation I)
Nutrients in Food and their bodily purpose XVI (Nutrients involved in Methylation II)
Nutrients in Food and their bodily purpose XVII (Nutrients involved in Methylation III)
Nutrients in Food and their bodily purpose XVIII (Nutrients involved in Methylation IV)
Nutrients in Food and their bodily purpose XIX (Methylation V and the Microbiota I)
Nutrients in Food and their bodily purpose XX (Methylation VI and the Microbiota II)
Nutrients in Food and their bodily purpose XXI (Superfoods: Wheatgrass)
Nutrients in Food and their bodily purpose XXII (Superfoods: Adaptogens)
Nutrients in Food and their bodily purpose XXIII (A look into our nutritional past Sir Robert McCarrison)
Nutrients in Food and their bodily purpose XXIV (Pregnancy: Nature vs Nurture vs Nutrition)
References/Acknowledgments :
- Essentials of Human Anatomy & Physiology 2000 Elaine Marieb
- Textbook of Medical Physiology 2006 Guyton & Hall
- Third Ventricle, Circumventricular organs, Pericyte, Vascular organ of lamina terminalis, A3V3 region, Subfornical organ, ADH, Aldosterone, median Eminence, Baroflex, Juxtaglomerular cells, Macula densa cells, Extraglomerular mesangial cells, Angiotensinogen, Dorsal nucleus of the vagus nerve, Supraoptic nucleus, magnocellular neurosecretory cells Wikipedia
- Glossopharyngeal nerve diagram google
- Conversion of Angiotensin I to Angiotensin II Erdos EG 1976 NCBI
- Control of blood pressure Lumen learning (Boundless anatomy and Physiology)
- General Overview of RAAS Khan Academy
- Glutamyl aminopeptidase 2013 Science direct
- Angiotensin receptor subtype mediated physiologies and behaviors:New discoveries and clinical targets Wright, Yamamoto, Harding 2007 NCBI
- High blood pressure ( Hypertension) medications RXlist
- Angiotensin II in the brain and the autonomic control of the kidney Edward Johns 2004
- Clinical relevance of local renin angiotensin systems Duncan Campbell 2014 NCBI
- Clinical perspectives and fundamental aspects of local cardiovascular and renal renin angiotensin systems Walmor de Mello & Edward Frohlich 2014 NCBI ( Frontiers of Endocrinology)
- Kallikrein-Kinin (KKS) and Renin-angiotensin-aldosterone system(RAAS)in primary Aldosteronism NIH ClinicalTrials.org
- Kallidin ScienceDirect
- Kallikrein-Kinin system ScienceDirect
Author : Eric Malouin