Introduction
In this part, concerning water as a nutrient, it is important to understand the biological mechanisms going on that filters and regulates blood volume, water reabsorption and waste excretion, the very duties of a remarkable organ the Kidney. The kidneys process the blood at a rate of 150-180 litres every 24 hours, and if you have lost one kidney this volume of filtration still has to be maintained, so one kidney is capable of filtering this amount of blood plasma, even if the remaining kidney has to expand a little…so as Dr B would say…wow..I love his passion for the unbelievable capability of the human body. So let us look a little closer into these organs.
The elimination of nitrogenous wastes Urea, Uric Acid, Creatinine

The kidneys have several duties to perform to maintain fluid balance and blood filtration within the body which include:
- The elimination of nitrogenous wastes Urea, Uric Acid, Creatinine
- Secretion, metabolism and excretion of hormones
- Gluconeogenesis
- Regulation of body fluid osmolality and electrolyte concentration
- Maintain water balance
- Maintain electrolyte balance
- Maintain acid-base (Ph) balance
- Regulation of arterial blood pressure
- Production of 1,25 dihydroxyvitamin D3 (Calcitriol)
Urea
So where does the nitrogenous waste come from ?.. first of all there is a biological process called the Urea cycle (one part of the methylation cycle set) which predominantly occurs in the hepatocytes ( Liver cells), and its purpose is to convert a toxic substance Ammonia, a resultant metabolite from amino acid metabolism from protein intake. Essentially ammonia is converted into Urea which can be easily excreted from the body, but ammonia excretion can do damage on its way out. This conversion is completed partially in the mitochondria and in the cytoplasm (the fluid space within the cell), The reason for this is, it requires energy to perform the chemical reactions, including the combination of carbon dioxide and ammonia ions, which produces Carbamoyl phosphate using 2 ATP/ADP molecules and an enzyme carbamoyl phosphate synthetase . Carbamoyl phosphate combines with amino acid ‘Ornithine’ to produce citrulline, which is then transported to the cytoplasm and combines with amino acid aspartate to form arginino succinate, requiring another ATP energy molecule. Another enzyme acts on the arginino succinate to form 2 molecules Fumarate and Arginine and finally arginine is enzymatically converted to Urea.
Uric Acid
Nucleic acids or purines (as in DNA,RNA) in the diet comes from many sources, including vegetables, fish etc, and when metabolised by the liver cells, it uses ATP energy to convert into Uric acid. Thus Uric acid is the end product of catabolism of purines in humans. Interestingly the Kidney reabsorbs most uric acid, to modulate its excretion into the gut rather than dump it rapidly in the urine. According to the research, an enzyme that exists in lower primates, called urate oxidase (Uricase) that breaks down uric acid into Allantoin does not exist in humans, despite the fact that we have the gene to express it, but it is non functional ( they say it was lost in early primate evolution ?). In lower primates, uric acid acts as a powerful antioxidant. Modulating the excretion rate from the kidneys maintains low concentrations of uric acid in the urine and plasma while the rest ( ¼ – ⅓) or more is degraded vicariously by bacterial flora that do possess uricase.
Gout
Having briefly discussed Uric acid in the previous paragraph we cannot forget the formation of gout which is a form of arthritis that affects the feet due to the buildup of Monosodium urate hydrate crystals. The cause is due to consuming excessive cooked foods that choke the normal excretion mechanism of the kidney, causing excessive uric acid to be dumped into the blood plasma, triggering inflammation from the crystal accumulation.
Creatinine
To understand where this waste product comes from, we need to revisit energy production within the mitochondria, specifically muscle metabolism and where muscle contraction during exercise source their energy from. The ATP energy source within the muscle fibres is only good for a few seconds so it needs other energy sources which include Creatine phosphate, Anaerobic Cellular respiration, and Aerobic cellular respiration.
Creatine Phosphate ( Phosphocreatine)
Creatine synthesis is produced in the kidney and liver, where it is transported to the muscles via the blood. An enzyme creatine kinase forms phosphocreatine by phosphorylating creatine which is used as an energy buffer in muscle and the brain by recycling ATP ( Adenosine Phosphate ). The kidney catalyzes 2 amino acids Arginine and glycine using an enzyme AGAT (L-Arginine:glycine amidinotransferase ) producing Guanidinoacetate (GAA), which is then transported to the liver adding a methyl group from amino acid Methionine by an enzyme GAMT (Guanidinoacetate N-methyltransferase) producing non phosphorylated creatine which is then transported to the muscle cells ( 95% of the body’s creatine is located in the muscle). Once inside the cells, an enzyme called creatine kinase transforms the non phosphorylated creatine into phosphocreatine. As we stated in part VIII ( Cellular energy production) it takes much more energy to relax a muscle vs muscle contraction so the muscle cell is able to create a short burst of energy that only lasts 15 seconds that is only capable of powering say a 100 metre sprint. Some athletes supplement creatine to enhance these short bursts of energy but there are concerns for their overuse.
Energy Production in muscle cells to perform exercise
 To maintain an exercise routine for say ½ hour-1 hour, the muscle must seek other sources of energy production, such as anaerobic cellular respiration which is fueled by the process of glycolysis delivering muscle energy slower than the use of creatine. The fuel used to drive this energy production can be glucose, directly derived from the blood, muscle glycogen ( a polysaccharide made of thousands of sugar molecules), inside the muscle tissue, which can only be liberated by a process called Glycogenolysis. Again, as discussed in Part VIII of this series we discussed the Electron Transport Chain (ETC) fuelled by glycolysis with oxygen, a process referred to as Aerobic cellular respiration, but anaerobic cellular respiration driven energy production, oxygen is absent, which can occur during intense exercise resulting in a brief depletion of oxygen, but it only delivers 2 ATP molecules, lasting only for a minute, which is able to sustain say a 400 metre race. This process is driven by lactic acid producing not only 2 *ATPs but the oxidised form of NAD ( NADH being the reduced form). The advantage with this type of fuel production, is the body can use either Pyruvate ( glycolysis), fatty acids or amino acids capable of delivering up to 36 ATP molecules. A point of note here is, the mitochondrial ETC actually prefers to burn fatty acids rather than glucose, so if glucose is in short supply, it is actually advantageous. However, since it requires a steady supply of oxygen it is a slower process, ideal for low intensity exercise like walking or light jogging. Finally, after an exercise routine, the body has to repay the oxygen debt, and the host may continue to breathe heavily for a short period or longer depending on the intensity of the exercise. Oxygen debt is ‘repaid’ back to the body from this recovery of heavy breathing, by converting lactate acid to glycogen to replenish the liver stores, the resynthesis of creatine to creatine phosphate, and to replace the oxygen in the myoglobin in the muscle (Oxymyoglobin). At this point the muscles may be fatigued and partially unresponsive to signals from the nervous system. It is speculated that this is a protective mechanism to avoid muscle damage, since the muscles experience a buildup of lactic acid, causing a more acidic environment, inhibiting efficient use of the muscle enzymes, and/or calcium leakage out of the cellular cytoplasm, and/or insufficient action potential to release acetylcholine at the neuromuscular junction. So these are typical values for nitrogenous waste products:
To maintain an exercise routine for say ½ hour-1 hour, the muscle must seek other sources of energy production, such as anaerobic cellular respiration which is fueled by the process of glycolysis delivering muscle energy slower than the use of creatine. The fuel used to drive this energy production can be glucose, directly derived from the blood, muscle glycogen ( a polysaccharide made of thousands of sugar molecules), inside the muscle tissue, which can only be liberated by a process called Glycogenolysis. Again, as discussed in Part VIII of this series we discussed the Electron Transport Chain (ETC) fuelled by glycolysis with oxygen, a process referred to as Aerobic cellular respiration, but anaerobic cellular respiration driven energy production, oxygen is absent, which can occur during intense exercise resulting in a brief depletion of oxygen, but it only delivers 2 ATP molecules, lasting only for a minute, which is able to sustain say a 400 metre race. This process is driven by lactic acid producing not only 2 *ATPs but the oxidised form of NAD ( NADH being the reduced form). The advantage with this type of fuel production, is the body can use either Pyruvate ( glycolysis), fatty acids or amino acids capable of delivering up to 36 ATP molecules. A point of note here is, the mitochondrial ETC actually prefers to burn fatty acids rather than glucose, so if glucose is in short supply, it is actually advantageous. However, since it requires a steady supply of oxygen it is a slower process, ideal for low intensity exercise like walking or light jogging. Finally, after an exercise routine, the body has to repay the oxygen debt, and the host may continue to breathe heavily for a short period or longer depending on the intensity of the exercise. Oxygen debt is ‘repaid’ back to the body from this recovery of heavy breathing, by converting lactate acid to glycogen to replenish the liver stores, the resynthesis of creatine to creatine phosphate, and to replace the oxygen in the myoglobin in the muscle (Oxymyoglobin). At this point the muscles may be fatigued and partially unresponsive to signals from the nervous system. It is speculated that this is a protective mechanism to avoid muscle damage, since the muscles experience a buildup of lactic acid, causing a more acidic environment, inhibiting efficient use of the muscle enzymes, and/or calcium leakage out of the cellular cytoplasm, and/or insufficient action potential to release acetylcholine at the neuromuscular junction. So these are typical values for nitrogenous waste products:
Urea, 12–20 g
Ammonia, 140–1500 mg
Creatinine, 14–26 mg/kg in men; 11–20 mg/kg in women
Uric acid, 250–750 mg
Kidney Filtration and reabsorption
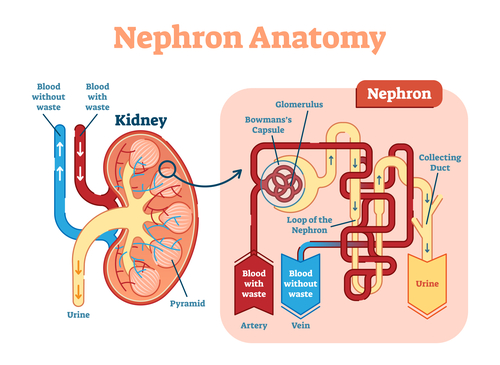
The functional engine of the kidney’s filtration and reabsorption system is the Nephron which is shown above. The diagram to the left depicts a ‘cutaway down the middle’ of a kidney showing the circular balls that are the renal medulla sections, three dimensionally, they resemble a pyramid shape, connecting the ureter or urine waste pipes. Inside these balls reside the small nephrons that number about a million in each kidney. The outer area surround is referred to as the renal cortex. The right of the diagram shows a ‘blow up’ view of one nephron. The red blood containing waste products are presented to the nephrons by an arcuate artery that branches off into an ‘Afferent arteriole’ (afferent = incoming or toward) which develops into a vast capillary system. The afferent arteriole enters a structure called the bowman’s capsule or Glomerular, set up as a series of loops, where the blood in this region is at high pressure that squeezes the filtrate out of the blood into the Bowman’s capsule and into the renal tubule (shown in yellow). Arteriole is a high resistant small arterial branch that leads into capillaries and it is this capillary bed not found anywhere else in the body that feeds the Glomerulus ( Bowman’s capsule). This tubule is known as the proximal convoluted tubule, at the start of the tubule in the bowman’s capsule proper, and the Distal convoluted tubule at the end just before entering the collecting duct. These 3 mechanisms, the Glomerulus, the proximal and distal convoluted tubules are referred to as the Juxtamedullary ( ‘near’ the medulla but still in the cortex) Nephron. The filtrate in the Bowman’s capsule/ proximal convoluted tubule contains H20, Salts ( NaCl etc), Bicarbonate (HCO3), H+(protons), Urea, Uric Acid, Glucose, amino acids and some drugs and poisons, while the distal end will contain NaCl, HCO3, some drugs and poisons. The filtrate is essentially blood plasma without blood proteins (larger molecules like red blood cells and large proteins are not filtered). The diagram below shows a little more detail:
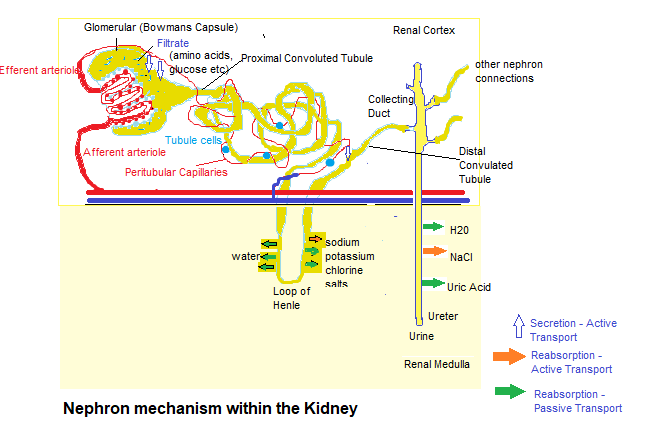
Shown in the diagram above, the blue arrows show secretion of poisons and protons from the blood into the renal tubule for final excretion. At the proximal/distal positions of the tubule it reclaims or reabsorbs substances that the body can use again, such as sodium chloride, bicarbonate, water, glucose and amino acids, and transports them into the peritubular capillaries that drain into the venous blood ( shown in blue ). The nephron extends from the renal cortex into the renal medulla forming a loop called the ‘loop of Henle’. The ascending portion of the loop uses passive and active transports ( active meaning the use of transport pumps fuelled by ATP, while passive transport refers to ions crossing cellular membranes via concentration gradients), to pump salts ( Sodium. Potassium, Chlorine ) into the renal medulla space, to make it a salty environment ( hypertonic = where there is more filtrate outside of the renal tubule as there is inside the renal tubule) making the ascending tubule permeable to salts and impermeable to water. The descending part of the renal tubule loop is only permeable to water, so by passive transport the water will leave the tubule to flow into the renal cortex space thus making this area the main location for water reabsorption. This flow of water must be passive because, although biological systems are good at pumping salts and ions, the proteins on the membranes are unable to pump out water. The long loop as it is designed, gives the nephron time for the water to be reclaimed. Finally multiple nephrons are attached to collecting ducts that take the waste out through the ureter, but even during this stage more water and more salts if reclaimable are reabsorbed into the medulla. Most of the filtrate ( approx 90%) is eventually reabsorbed.
Conclusions
What we have not discussed is a piece of the renal tubule located where the thick ascending limb meets the distal convoluted tubule, where lies a pack of specialised cells that line the wall of the distal tubule called the Macula densa that sense sodium chloride concentration, playing a part in the renin-angiotensin-aldosterone axis, that regulates blood pressure and blood volume, in addition to acid-base balance. We will cover these topics in more detail in the next chapter of this series.
PETE “If PG&E messed with our water, why would
they bother saying anything about it to
us? Why not just keep quiet about it?”
ED “To establish a statute of limitations.
See, in a case like this, you only have a
year from the time you first learn about
the problem to file suit. So PG&E
figures, we’ll let the cat out of the bag
— tell the people the water’s not
perfect; if we can ride out the year with
no one suing, we’ll be in the clear
Forever.”
Quote from Erin Brockovich Movie 2000
Check out other Articles in this series:
Nutrients in Food and their bodily purpose I (Phenols)
Nutrients in Food and their bodily purpose II (Lignans, Triterpenes, Phytosterols, Carotenoids & Fats)
Nutrients in Food and their bodily purpose III (Phenolic acids, sulphur, sulphides,sulphoxides )
Nutrients in Food and their bodily purpose IV (Glucosinolates, Sulforaphane, Indole-3-Carbinol)
Nutrients in Food and their bodily purpose V (Lipid distribution, absorbed fats, Criciferous Veg)
Nutrients in Food and their bodily purpose VI (Nutrients required for Liver Detox)
Nutrients in Food and their bodily purpose VII (Seeds & the Omega Fatty Acids)
Nutrients in Food and their bodily purpose VIII (Nutrients required for cellular energy production)
Nutrients in Food and their bodily purpose IX (Water I Properties and Body fluids)
Nutrients in Food and their bodily purpose X (Water II Cellular Hydration)
Nutrients in Food and their bodily purpose XII (Water IV Blood pressure, Blood volume regulation)
Nutrients in Food and their bodily purpose XIII (Water V Body Fluid Dysfunction
Nutrients in Food and their bodily purpose XIV (Dental Nutrients)
Nutrients in Food and their bodily purpose XV (Nutrients involved in Methylation I)
Nutrients in Food and their bodily purpose XVI (Nutrients involved in Methylation II)
Nutrients in Food and their bodily purpose XVII (Nutrients involved in Methylation III)
Nutrients in Food and their bodily purpose XVIII (Nutrients involved in Methylation IV)
Nutrients in Food and their bodily purpose XIX (Methylation V and the Microbiota I)
Nutrients in Food and their bodily purpose XX (Methylation VI and the Microbiota II)
Nutrients in Food and their bodily purpose XXI (Superfoods: Wheatgrass)
Nutrients in Food and their bodily purpose XXII (Superfoods: Adaptogens)
Nutrients in Food and their bodily purpose XXIII (A look into our nutritional past Sir Robert McCarrison)
Nutrients in Food and their bodily purpose XXIV (Pregnancy: Nature vs Nurture vs Nutrition)
References/Acknowledgments :
- Essentials of Human Anatomy & Physiology 2000 Elaine Marieb
- Textbook of Medical Physiology 2006 Guyton & Hall
- Phosphocreatine, Glycogenolysis, Macula Densa, Juxtamedullary Wikipedia
- Renal excretion of uric acid in normal and gouty man 1965 Alexander Gutman MD
- Muscle Metabolism 2015 Youtube AnatomyZone
- The kidney and the Nephron Khan Academy
- Movie quotes from Erin Brockovich Screenplays for you
Author: Eric Malouin