Introduction
Obesity, without a doubt is a chronic health condition that poses a dangerous risk to many biological functions in the body, and has a tremendous psychological effect to most, who just want to be a normal size, and make tremendous efforts to lose weight but can’t. The health care system that is supposed to be there to help such people, fail, and fail miserably by trying to short circuit the natural functions of the body. Their dark age scientific methods include the ‘bacon slicer’ liposuction, gastric bands, mouth zips..lol and God knows what else. Or they suggest that you change your diet and exercise…just like that… because they know absolutely nothing about obesity; they don’t put any time aside to research the condition and are completely clueless about weight loss and how it can be achieved. In this series of articles I will explain how you can get your health back, and then how to achieve successful weight loss without busting a gut in the gym trying to shed some pounds with false information that will leave you discouraged and not lose anything..except money. It requires effort people..this is not the quick fix cover up solution that conventional medicine can only provide; it takes belief, lots of encouragement from people around you, sheer will power but above all, the knowledge to achieve your goals.
Obesity Pathogenesis

I don’t think it’s any surprise to most people that Obesity is an unhealthy condition of the body caused by physiological, chemical and psychological imbalance fuelled by nutrient deficiency and usually poor diet, and fuelled by a sedentary lifestyle. Its pathogenesis includes genetics, environment, metabolism and endocrine factors. Thats is a lot of ‘stuff’ to fix, but the good news is that improving lifestyle, diet and correcting dietary intake and detox, most of the associated physiological problems will be corrected by the self healing properties of the body. Then it’s time to work for the body. As I said before:
‘ OBESE PEOPLE ARE SICK AND UNHEALTHY, HOW CAN YOU POSSIBLY TALK ABOUT EXERCISE UNTIL THE PERSON BECOMES HEALTHY AGAIN…SO HEALTH FIRST THEN EXERCISE’
Exercise is beneficial since this will activate the fat burning hormones and deactivate the fat storing hormones, but more of this later.
What obesity does to the human body

Massive macrophage mobilisation in adipose tissue during obesity conditions
According to the research, adipose tissue normally is made up of 50 % adipocytes, fibroblast cells that constitute connective tissue such as collagen, endothelial cells that line the inner surface of blood vessels and lymphatic vessels, preadipocytes which are undifferentiated fibroblast cells that form to make adipocytes, and finally macrophage immune cells which make up approximately 5-10% of the total adipose cellular tissue. In obesity an inflammatory condition exists causing an accumulative death of many adipocytes and the recruitment of many macrophage immune cells which changes the adipose macrophage density from 5-10% to 50-60% and they are joined with other immune cells including dendritic cells, mast cells, neutrophils,, B cells, and T cells all contributing to adipose tissue inflammation in a futile attempt to fix the problem. The role of the macrophage army is the clearing of cellular debris and efferocytosis ( the burying of dead cells), immune surveillance and their attempt to resolve the inflammation and trying to achieve adipose tissue homeostasis. Although macrophages play a key role in maintaining adipose tissue homeostasis, at the same time they fuel adipose tissue inflammation upon the development of obesity, confirming biological imbalance.
The marvel of Macrophages
I believe that my previous discussions on the immune system probably gave you the impression that B and T cells led the charge in terms of innate immunity response to pathogenic invasion and at some point macrophages are recruited to kill pathogenic bacteria and clean away the bacterial debris, which indeed they do. However, Macrophages are much more important than that, since they must be first responders to an attack, if you consider that one brutal pathogenic bacterium can become the same mass as a human in 4 days..that is incredible proliferation and certain death to a human host. Consider also that a T or B cell can only become 16 cells in 4 days..hardly an effective defence, which is why the M1 Kill Macrophage is crucially important and engaged immediately if the host is to have any chance of survival. This also confirms the tight function between innate and adaptive immunity systems, where the innate immunity must always be our ( and in all animals) first line of defence that immediately springs into action upon the detection of a threat, rapidly mobilising elite macrophage kill units that destroy pathogens on the spot within hours to prevent mass pathogenic proliferation.
In conjunction with the M2 Repair Macrophages the M1 Kill Macrophages are the essential core of the immune system where M1 promotes inflammation and M2 inhibits inflammation. M1 Kill macrophages use L-Arginine amino acid as a precursor to the production of Nitric oxide (NO) and its enzymatic by product Citrulline as its ‘death ray’ for pathogenic bacteria. On the other hand depending on the cytokine immune signalling the Macrophage could act as an M2 repair/proliferation medium producing ornithine from arginine and its enzymatic by product urea to heal tissue which typically occurs during wound healing. Remarkably, a wound induces macrophage M1 intervention that spray NO for 2 days to kill off any potential pathogen and sterilize the wound area and then it turns its attention to healing the wound using ornithine. This explains why the mass mobilisation of macrophages within the adipose tissue, since the obese condition is causing abnormalities by increasing the size of the adipocytes. However, the obesity perturbation is too widespread and continuous for the macrophages to put the inflammation fire out because the host is continuously fuelling the fire.
Endoplasmic Reticulum (ER) stress
Within the obese condition, adipose cells are subjected to endoplasmic reticulum(ER)* stress causing folded proteins to become unfolded ( like sending a parcel through the post that has become damaged and its contents are exposed), but the cell has certain mechanisms to repair the damage referred to as the UPR (Unfolded Protein Response)**, but if this fails then the cells are marked for death or apoptosis which the macrophage is responsible for disposal. Additional stress on the adipocytes caused by obesity is the unnatural enlargement (Hypertrophy) of the cells and proliferation of cells ( hyperplasia). Having said all that, however, the mechanisms that induce ER stress by obesity, and ER stress relationship with chronic inflammation is still not that well understood, or least that was the position in 2012. Equally it has been shown in mouse experiments that Free Fatty acids *** that are elevated in obese patients had the potential to cause ER stress. In a study conducted by Noritaka kawasaki et al in 2012 they investigated Obesity induced endoplasmic reticulum stress causing chronic inflammation in adipose tissue and found by inserting chemical chaperones****it suppressed the inflammatory response and improved insulin signalling. This same study confirmed a link between the increase of free fatty acids in obese patients also increased the ROS ( Radical oxygen species ) within the ER oxidising nascent (a protein as it is being formed by a ribosome before it folds into its biological active shape) proteins causing protein misfolding by interfering with the concentration of calcium in the ER lumen.
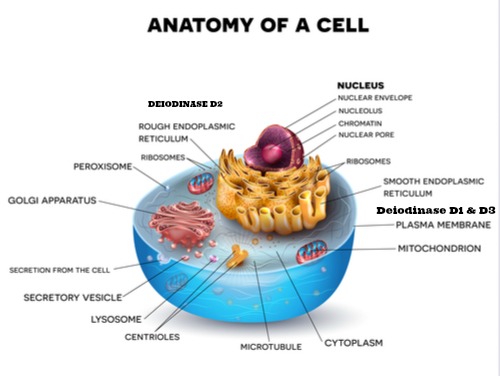
*The endoplasmic reticulum as shown the cell diagram is the site where proteins are synthesised and packaged (folded) and sent to the cells transportation system ( cellular post office) called the Golgi apparatus that either sends the ‘protein parcels’ internally or externally for cell signalling purposes.
** Protein molecules are composed of widely dissimilar elements or heterogeneous unbranched chains of amino acids which must be coiled and folded into specific 3 dimensional shapes so as they assume their biological function
***Free fatty acids: dietary fat is normally in the form of Triacylglycerol (TAG) consisting of 3 fatty acids linked to a glycerol which is then broken down with water (hydrolysed) by pancreatic lipase that liberates the fatty acids and monoglycerides. The fats are further broken down by bile released into the duodenum by the gallbladder creating micelles which are small enough to be absorbed, along with fat soluble vitamins and cholesterol that are also contained in the tiny micelles. Once absorbed by the enterocytes on the microvilli, the fatty acids and monoglycerides are reformed as TAGs and packaged together with the vitamins and cholesterol inside Chylomicrons, a lipoprotein transport that can travel the bloodstream via lymphatic vessels like a lipid boat delivering its cargo to cells. The fatty acids known as triglycerides can be used to fuel cellular energy production as is done by the liver that also stores triglycerides that are broken down into fatty acids to use as fuel by the cells. In addition the liver can perform gluconeogenesis that converts amino acids into glucose, as well as the ability to break down glycogen and converted into glucose, stimulated by a hormone Glucagon secreted by the pancreas, in response to low blood glucose levels, to achieve biological stability which normally happens under intense exercise.
**** Chemical chaperones that can be amino acids Arginine or Glycine that have the ability to enhance folding and general stability of proteins. For example chemical chaperones have been used to treat Cystic fibrosis(CF) by promoting a mutant (gene) CFTR (Cystic fibrosis transmembrane conductance regulator) membrane protein, responsible for transportation to the plasma membrane. As I have stated before assuming CF is the responsibility of a mutant gene, in this case the CFTR gene, it is questionable since Dr Joel Wallach proved back in 1978 that CF is caused by a selenium deficiency found in primates.
Insulin resistance (IR)
According to medical science, adiposity growth causes hypertrophy and hyperplasia and a diverse variation in different adipose tissue depots, since tissue expansion in some depots increases IR risk and lower in others, pertaining also to diversity in individuals. It is believed that the presence of hyperplasia ( abnormal growth) the risk of IR is diminished. Although studies have discovered that insulin sensitivity is decreased in muscle cells (myocytes) in obese individuals, hypothesised to be caused by excess lipids that downgrade insulin signalling. It is also hypothesised, that it is the impaired insulin stimulated glucose transport, in addition to impaired inhibition of lipolysis (the breakdown of fats and other lipids by hydrolysis to release fatty acids), that cause insulation resistance within the obese condition. It has also been suggested that hypoxia which is defined as oxygen demands that exceeds oxygen supply in adipose tissue, has a correlation with the excessive size of the adipose tissue that has expanded due to obesity. Because of the additional weight around the neck this can cause oxygen inhalation restriction related to sleep apnea which has a bearing on the availability of oxygen. At least 85-90& of obese individuals also suffer from insulin resistance. Despite the many studies, the evidence appears to identify symptoms of obesity but not causal facts, which is also confirmed by the researchers themselves. At this point, despite those who believe that obesity causes insulin resistance, their is little evidence to suggest this, in fact there are many studies like the one conducted at Laval University Quebec Canada. In this particular study 31 obese women completed a 6 month aerobic exercise program. Although among the group most lost 6 pound of body fat, but 11 of the 31 actually gained weight, but all of the group obtained cardiovascular improvement and their insulin levels concluded that the exercise improved their insulin levels not weight loss. Insulin resistance can be easily reversed by diet wether you are fat or thin. The Pritkin longevity centre in California have found similiar findings that diet and moderate exercise like walking is key to improving health, applicable to all shapes and sizes.
Conclusions
We have established that obese individuals, most of which are not gluttons, and they hate to be obese, and I agree with the statement by Robert Pool in his book Fat: fighting the obesity epidemic that people are eating normally in an abnormal environment. Our weight regulating system or homeostasis energy balance system was designed for the Hunter/Gatherer environment where the human race searched for food like our animal and bird cousin species, and they would walk miles every day foraging for food. Today, however, food is plentiful and we don’t have to go far to get it, and if it is far we have transportation. Today’s modern world is full of labor saving appliances, taking manual work away from the human, and of course we have an abundance of man made processed food and fast food that has been specifically engineered by food scientists to highly stimulate our regulatory food intake processes and purposeful manipulation of the reward/hedonistic controls of the brain. Although this man made food is poisonous to the body, because we don’t have the ‘blueprints to metabolise it, our taste and smell sense the insatiability of the food causing addiction. In the next article I want to discuss our biological energy balance system so you can appreciate the intelligence of the body that contains multiple controls to avoid the body getting out of control.
References/Acknowledgments :
- Adipose tissue macrophages : going off track during obesity Boutens & Stienstra 2016 NCBI
- Digestion and Absorption of fats Conjoint 401-403
- Obesity induced endoplasmic reticulum stress causing chronic inflammation in adipose tissue Noritaka kawasaki et al 2012 Scientific Reports
- Mechanisms of insulin resistance in obesity Jianping Ye 2013 NCBI
- Regulation of obesity and Insulin resistance by hypoxia inducible factors Jae Jun Ban et al 2014 NCBI
- The physiology of glucagon-like peptide 1 Holst 2007 NCBI
- Mechanisms of Action of GLP-1 in the Pancreas Doyle & Egan 2007 NCBI
- Incretin hormone Diabetes self management 2013
- Fat: fighting the obesity epidemic book Robert Pool 2000
Author : Eric Malouin