Introduction
We have discussed some common autoimmune conditions including fibromyalgia, rheumatoid arthritis, allergies, and associative ( in terms of causal origins like toxic overload) asthma and chronic cystitis. If you have read the previous chapter in the series you have a fair functionalawareness of the immune system, but this immense defense force comprised of 2*10 power 12 ( 2 trillion) lymphocytes split into 2 huge battalions of T and B cells. The body is capable of generating 10 power 7 ( 100 million) specific antibodies. Within the complement system(antigen surveillance within the bloodstream), each B cell has somewhere in the region of 10 power 5 ( 1 million ) identical specific antibodies located on its cell surface, the ‘antigenic universe’ scanned within the humoral environment is achieved by 10 power 17 (can’t count that high) cell bound receptors. The number of lymphocytes in the blood ( estimated 10 power 10) have a mean residence time of approx 30 minutes which results in an exchange rate of 50 times/day. Thats a lot of movement and an unbelievable coordination task to keep the surveillance armies functioning, not to mention the coordination necessary to respond to a foreign invasion, and to keep the troops recycled and trained coming out of the thymic training school and the bone marrow. However, all this ‘firepower’ can only work if the body is balanced and working in harmony, otherwise you have a very powerful arsenal that can only fire blanks. In this part I want to discuss the Thyroid gland and how it becomes affected by autoimmunity and to discuss other problems that can occur.
The purpose of theThyroid

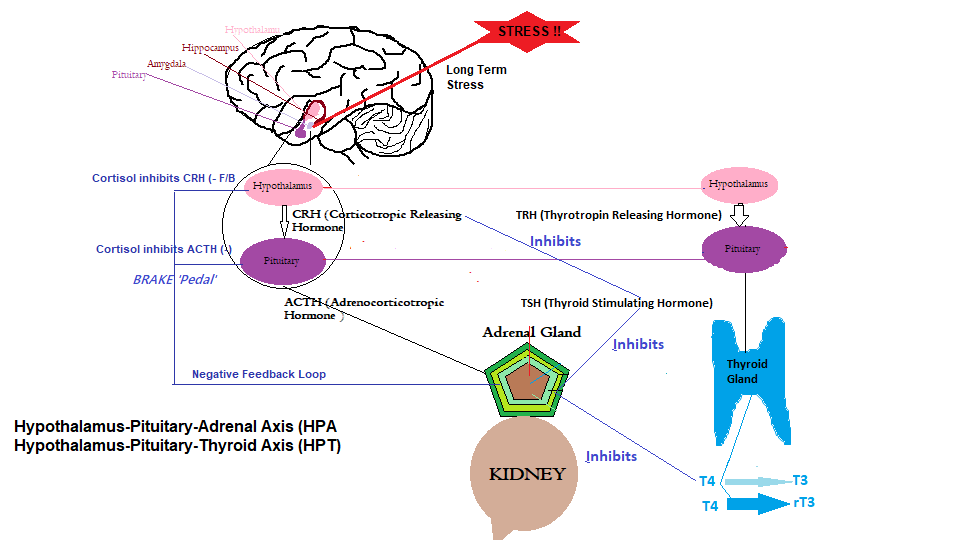
The purpose of this small gland (about 2.5 inches wide) regulates the burn rate of food to produce energy, controls tissue production for hair and nail growth, acts as our internal thermometer, and cholesterol level regulation ( secreted active thyroid hormone (T3) breaks cholesterol into more LDL particles ). How well you feel is partially under the control of the Thyroid since it can regulate serotonin levels in the brain, increase cardiac output as needed and of course control basal metabolism ( at rest ) regulating functions that include breathing, blood circulation, body temperature, cellular growth and muscle contraction. The thyroid works like this, whatever the host is doing or experiencing, if its cold and you need to increase your heart rate, and/or your need to get things moving for sex etc then the HPT (Hypothalamus-Pituitary-Thyroid) axis kicks in. This is a relatively simple feedback mechanism involving the hypothalamus that senses the circulating levels of T3/T4 in the blood, and if too low it will send a downstream signal thyrotropin-releasing hormone (TRH) to stimulate the Pituitary to signal stimulate thyroid-stimulating hormone (TSH) the thyroid to manufacture more T3/T4. Through the feedback circuitry from the thyroid back to the hypothalamus, regulation is achieved turning off the hypothalamus signal once blood levels of T3/T4 have normalised.
Hyperthyroidism (Graves)/Hypothyroidism (Hashimoto)

I am sure many out there are aware of Hyperthyroidism. This is where the thyroid goes into overdrive and over produces its hormone Thyroxine (T4; tetraiodothyronine; thyroxin). This phenomena is referred to as ‘Graves disease’. Thyroxine is known as T4 and is actually the storage form of this thyroid hormone, which is converted by the Liver and kidneys when it arrives from the bloodstream to its active form T3 or Triiodothyronine. In actual fact this thyroid hormone release mechanism is designed to produce approximately 20% of the active T3 and 80% T4 which have half lives of 2.5 days and 6.5 days respectively. This ratio is maintained to compensate for the various tissue sensitivities. Another condition is called Hashimoto’s Thyroiditis or Hypothyroidism which in this case involves an inefficiently functioning thyroid to the slow destruction of the thyroid gland through constant bombardment from the immune system. Interestingly some people may suffer both conditions that flip flop between the two,which I imagine is quite uncomfortable since Hyperthyroidism ( Graves ) express symptoms of : Appetite fluctuation, insomnia, fatigue, diarrhea, heart palpitations, heat intolerance, increased sweating, irritability, menstrual cycle fluctuation, cognitive issues, muscle weakness, nervousness, breathing issues, paralysis, vision issues, weight fluctuation, itching/hives, blood sugar fluctuations,and hair loss. Hypothyroidism (Hashimoto) expresses: Fatigue, weakness, weight fluctuation, dry hair, hair loss, cold intolerance, constipation, depression, irritability, memory loss, menstrual cycle fluctuation, decreased libido. As I said, uncomfortable; one week your constipated and cold, next week you hot and have diarrhea, but at least muscle weakness, fatigue stays constant.
Physicians to the rescue..Again
So, what’s going on ??. How is the poor physician going to deal with this problem..
”now let me see, what do I have here…radioactive iodine”..
“What !!,… radioactive ?”,..No i will take some sea kelp”
“methimazole….throttles the thyroid..side effects..hm..ok it puts a target on your back for infection..and..liver inflammation..nothing too drastic…. or we can prescribe propylthiouracil…side effects..er..same thing really with an added benefit of excessive bleeding and very rarely fatal liver failure..don’t worry I am sure you will be ok”….. We could of course take the thyroid out……what is that new tv series..’Altered carbon’……and there is of course beta-blockers”..(.I believe we wrote about this in the article ‘Microbiome and Disease Part 1 concerning the rehydration axis; the Renin-angiotensin-aldosterone system). This is the current allopathic treatment for Graves disease and for Hashimoto’s disease “
“We have a synthetic T4 Hormone called levothyroxine Sodium…side effects..hm..Chest pain, heart & pulse rate increases, excessive sweating, heat intolerance, nervousness, headache, insomnia, diarrhea, vomiting, weight loss, fever”…..
” Wait a minute you are going to prescribe a drug that will convert my Hashimoto symptoms to look like Graves symptoms..are you nuts”.
Testing for antibody manufacture
To distinguish between both conditions. In Hyperthyroidism (Graves) thyroid stimulating antibodies referred to as Thyroid stimulating immunoglobulins (TSI) are in abundance, whereas In Hypothyroidism( Hashimoto) thyroid peroxidase auto antibodies (TPO) and TSI are both High. So what ? you may ask…..well foolishly in the case of Hashimoto’s disease the prescribed medicine is managing the Thyroid Stimulating Hormones (TSH) using Hormone replacement therapy while the immune system is gradually destroying your thyroid gland, and giving you Graves look alike symptoms..confused..yep..so am I. But you haven’t heard the best of it, most people with intermittent low levels of TSH are not diagnosed with full blown Hashimoto’s disease, but with the HRT they end up with it anyway and by then the immune system is quite happily munching away at your thyroid.
Attack on the thyroid gland
So people listen up….as Dr Bergman stated in his excellent video on this subject..”This is not a problem with the Thyroid”..indeed it is not, it is a problem with the immune system..THAT’S WHY ITS CALLED AUTOIMMUNITY..DAH…I feel like we have spun around 360 degrees in a northly direction. In 2017, four scientists carried out a study using several patients with hashimoto’s disease and found imbalances in T cell related transcription factors concerned Th1,Th2 and Th17. If you remember we discussed how important Th1( overall infections of the body) and Th2( humoral or liquids of the body including the bloodstream) need to be balanced to maintain immune system integrity. As they concluded after the study they stated that “correction of these balances would be therapeutic”. The study also uncovered some other clues to immune system dysfunction. Significantly elevated expression of T-bet transcription Factor. T-bet (also known as TBX21) has been described as a bridge between the innate and adaptive immune system by coordinating Th1 immune responses using genetic control regulating immune cells used in both branches of the immune system. At the center of a Th1 inflammatory response (Infection) is the T-bet that is a critical regulator of T Cell differentiation(Th1,Th2,Th17 ), that induces Interferon-γ a cytokine messenger. Interferon-γ is critical for both branches of the immune system in defending against Viral invasion and some bacterial infections. Destabilising interferon-γ induction by overexpression is associated with autoimmunity (autoinflammation). Another clue that indicates the immune system is not doing its job, is, within this study they found FOXP3, a protein involved in T-regulatory cells that is responsible for turning down the immune system, malfunctioned. stating that it was significantly diminished.
Thyroid conversion issues
Just to be clear the autoimmune conditions described above are not the only ones that affect thyroid function since the liver/gallbladder has the main conversion engine for T3, so to in the kidney, and the thyroid itself but to a lesser degree, but importantly conversion also occurs in the Pituitary and the GI Tract ( the gut).. Yet another example not to implicate the target organ (the thyroid) as the dysfunctional organ within the ‘grand scheme of things’, For example, Triiodothyronine (T3) and its precursor thyroxine(T4) are ‘iodinated’ ( needs dietary iodine to function) substances that actually influence gene expression in virtually every tissue. Three Deiodinase enzymes (D1,D2,D3) are involved in the activation/deactivation and conversion of T3 and T4. D1 converts inactive T4 into T3 the active form throughout the body.
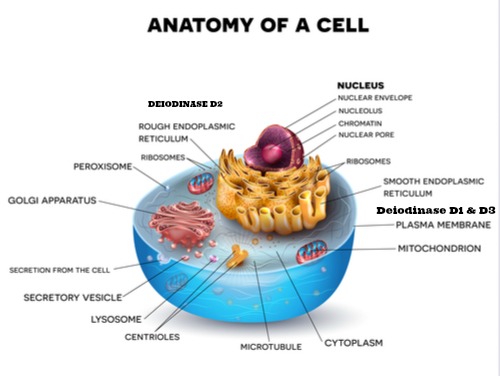
Deiodinase enzyme D2
As part of the balancing act or should I say the ingenious functional design of the body, the pituitary also converts T4 to T3 using D2 which is unaffected by negative conditions that may prevail in the body unlike the D1 conversion in the liver and cells. At the cellular level D1 and D3 reside in the plasma membrane while D2 is located in the endoplasmic reticulum ( as shown in the diagram ) and once the T4 arrives in the cell the converted T3 by D2 can directly enter the nucleus and interact with thyroid receptors.
Deiodinase enzyme D3
This enzyme is normally not expressed under normal healthy conditions. It is active in the neonate and placenta to protect the developing embryo from excess thyroid activity. It does become active when the body decreases the metabolic rate in response to host starvation or restrictive food intake, critical illness, inflammation. In hyperthyroidism (Graves condition or thyroid overdrive) it increases in an attempt to throttle back thyroid activity, and decreases in hypothyroidism ( Hashimoto’s condition or underperforming and gradual thyroid destruction), in order not to impede normal T4/T3 conversion as you would expect. Remember D3 takes T4 out of circulation, thus reducing the T3 availability by converting it to reverse T3 (rT3).
Cellular Hypothyroidism
What most physicians are not aware of is the transport of T3 and T4 across the cellular membrane is not passive, but requires energy to cross it, which means that any negative condition ( autoimmune disease, mitochondrial dysfunction etc) will affect the transport of these hormones into the cell. This aberrant situation is known as Cellular Hypothyroidism. So during these inflammatory, stress and/or ‘disease’ events, more reverse T3 is made so you would expect elevated levels of rT3 in the plasma but low levels in the cell, which is useless since rT3 is incapable of delivering oxygen and energy to the cells. In fact rT3 blocks the effect of T3 from binding to receptors disabling its function, and as a result D1 is converting for nothing, as well as D3 blocks the cellular absorption of T3 and T4 anyway.
T3 Metabolites and the Gut connection
So not only does inflammatory conditions affect these hormones but an unhealthy gut also affects their operation. Up to now we have discussed T3,T4 and rT3. In the opening paragraph of this section I stated that the thyroid hormone release mechanism is designed to produce 20% of the active T3 and 80% T4. The T4 is not all converted to T3. Approximately 40% of T4 is converted into rT3, 20% into T3 and 20% gets converted into T3 Sulphate and T3 Acetic acid. It is these 2 metabolites (T3 Sulphate and T3 Acetic acid) that find their way into the gastrointestinal tract where they are converted to T3 by bacteria that produce the necessary sulfatase enzyme to complete the conversion. So the body comes to the rescue again with this neat contingency plan. If D1 converted T3 is low, due to say adrenal stress, than at least 20% can be converted in the GI Tract. However, it is very possible that the condition affecting D1 converted T3 (dysbiosis) could also affect the bacterial conversion as well.
The Detective

When Conan Doyle created the Sherlock Holmes (1859-1930) character he included another detective of another kind Doctor Watson. Doctors in his day did not have an arsenal of poisonous chemical substances to inflict on the general public except for morphine and laudanum ( an opium (1%) and codeine mixture), so they had to rely on their deduction skills to treat the sick. Today conventional medicine have high tech gadgets, expensive imaging machines, monitors and all of the accumulated science of 100 years at their disposal. All of the scientific work on the microbiome including the 5 year study in 2007 to sequence the microbiome, the days of Theodor Escherich (1857-1911) who found E Coli in the intestinal flora of healthy children, and the plethora of nutritional science is all simply archived non referenced data in the eyes of conventional allopathic medicine, allowing crucial clues to just slip by into oblivion. This modern day behaviour, is robbing conventional physicians the chance to become real modern day doctor Watsons.
Measurements and tests to diagnose thyroid dysfunction
Even today thyroid functionality testing as to diagnosing hypothyroidism is rudimentary at best. TSH ( Thyroid Stimulating Hormone or Thyrotropin) that is released by the pituitary to stimulate the thyroid into producing T3/T4 is measured. This test simply determines if the thyroid is a little flaky since it will increase if the thyroid is not producing enough and decrease if there is enough floating around in the blood. Unfortunately people who complain of the symptoms as described above for the most part will have normal ( according to WHOM?) readings ( range 0.5-4.5). What the conventional physician can order in terms of blood tests are the following :
- Total T4 and Total T3 to establish a baseline ( I believe most doctors measure this anyway )
- Free T4 that measures how much of the hormone that is available to enter the cell ( since bound T4 to a protein is necessary to transport it in the blood stream because most hormones are fat soluble and are incapable of cell entry while bound to the transporter protein). This measurement can actually be confirmed by measuring T3 uptake ( this measures the amount of binding sites that are available for Free T3). Then the Free T4 can be multiplied by the T3 Uptake value which should come close to the measured Free T4
- Free T3 can be measured to get an idea of free T3 unbound that can enter the cell
- Reverse T3 can be measured to gauge an idea of how much T3 is deactivated.
Remember what we stated above a healthy thyroid is designed to produce 20% of the active T3 and 80% T4. Approximately 40% of T4 is converted into rT3, 20% into T3 and 20% gets converted into T3 Sulphate and T3 Acetic acid for bacterial conversion into Free T3. The table below shows roughly the established reference values that will determine the treatment of the thyroid in conventional medicine.
| Thyroid Function Tests
Affected by TBG Corrects for high/low values of TBG Roughly indicates potential Peripheral T4/T4 conversion problems If low TBG binding capacity is high and vice versa |
Thyroid Function Testing
|
|||||||||||||||||||||||||||||||
ug/dL = micrograms per deciliter
ng/dL = nanograms Per Decilitre
mIu/mL = milli-international units per milliliter
U/mL = units per millilitre
TRH = thyrotropin-releasing hormone stimulating signal from hypothalamus to pituitary
TSH = thyroid-stimulating hormone stimulating signal from Pituitary to thyroid
TBG = Thyroxine-binding globulin binding protein to transport hormone in the blood to its cellular destination
Thyroglobulin = Protein precursor for thyroid hormone and is measured here as a biochemical thyroid tumor marker, but defined to be a nonspecific marker if the thyroid is inflamed or enlarged..as I said a potential tumor marker.
If we don our detective deerstalker you need all of these test measurements to determine whats going on, so a high Total T4 with low Total T3 and high rT3 values than this would indicate that rT3 is sitting on the cellular binding sites inhibiting T3 function. This typically would be caused by stress, trauma,chronic dieting, toxicity, infection or other medications. If on the other hand T4 is low this could indicate nutrient deficiency such as iodine, or iron, low stomach acid that may be causing malabsorption of selenium, zinc or cofactors that are required from Vitamins A,C,E and amino acid tyrosine and of course gut health. Therefore the glaring clues are nutrient deficiency and/or toxicity due to lifestyle and dietary habits
“ So Watson what other clues can we glean from this crime that will verify our suspicions?”
Other clues I – Parathyroid and Calcium
Since the thyroid communicates with the parathyroid gland ( 4 tiny rice grain size glands located behind the thyroid) it releases a hormone called Calcitonin which is an inhibitory signal to reduce blood calcium levels. This is an opposing signal to the parathyroid that regulates calcium levels in the blood. Since calcium is a crucial mineral for blood clotting, nerve impulse transmission, muscle contraction, cell membrane stability and cell metabolism etc, the parathyroid maintains a fairly tight calcium level in the blood, and if it falls, it will secrete a hormone called PTH. This hormone affects 3 other body locations, the bones, the small intestine and the kidneys. It triggers the body to leach calcium and phosphorous from the bones, in the intestine to enhance calcium absorption in concert with Vitamin D3 and in the kidney to prevent recyclable calcium from being expelled from the body through urine. Since the parathyroid doesn’t care ( biologically speaking) where it gets its calcium from, the body has to control how much calcium is leached from the bones to prevent osteoporosis, so its uses the thyroid to apply the brakes. If there is dysfunction in the thyroid, potentially the brake pedal is not going to work, the body will go ahead and leach the calcium from the bones and the malabsorption of calcium can occur and calcium deposits will begin to show up as well as the risk of calcium stones in the kidney.
Other clues II – Oxidative stress
‘ROS > Cellular antioxidant capacity = Oxidative stress’
Cellular Antioxidant enzymes
Thyroid hormones are involved in regulating basal metabolic states ( the minimum amount of energy required to sustain vital functions in the human body during a resting state ), and oxidative metabolism ( the use of oxygen to produce energy from carbohydrates, referred to also as aerobic respiration). As a by product from oxidative metabolism Reactive Oxygen Species (ROS) or Free Radicals are produced which can have a damaging effect on the body, if it is not kept in check by antioxidant activity, to the point of oxidative stress. This potentially can damage crucial building blocks of the body such as proteins, lipids and DNA. Luckily for us the functional design of the body includes free radical scavengers inside the cell to absorb these damaging particles. These various antioxidant enzymes include Catalase, Superoxide dismutase and Glutathione peroxidase (used to convert hydrogen peroxide into harmless water for example).
Glutathione
The master antioxidant Glutathione (GSH) is made from 3 amino acids Cysteine, Glycine and Glutamate and the highest concentration is in the liver, which gets transported to other cells. Since Glutathione becomes oxidized itself, through its antioxidant activity, Glutathione reductase enzyme reduces it back to its non oxidized state, since glutathione is a Redox molecule itself. Within the mitochondria of the cell where oxidation occurs, is also the eventual home of the thyroid hormones. During the thyroid hormone synthesis process, oxygenated water (hydrogen peroxide H2O2) is constantly being produced which is toxic to the cell. The molecular mechanism of iodination to achieve the final useable hormone products by the cell create free radicals as intermediaries during the successive stages, as an example H2O2 is converted into thyroperoxidase (TPO) forming a compound that oxidises iodine. This is why a powerful antioxidant molecule is essential to be present. Selenium is also a requirement for the T4 to T3 conversion since the deiodinase enzymes ( D1,D2,D3) contain selenocysteine ( the 21st amino acid ?) as well as Glutathione peroxidase. So depletion of Glutathione can occur if the host has a lot of cellular toxicity and high oxidative stress. Other vitamins are required like some B vitamins including B1 and B6. Methylation, a topic we covered in the 90 essential nutrient articles is also key in terms of cellular function requiring other nutrients like folate acid and methionine..
The Adrenal Stress connection

Conversion while under physiological stress and chronic conditions
When the body is in stress mode including depression, dieting,leptin resistance ( leptin is a signal sent from the adipose tissues to inform the hypothalamus that the host is full and should cease eating), insulin resistance, obesity, diabetes, autoimmune inflammation, and toxicity, the body down regulates D1 diminishing the conversion. It also increases reverse T3, and its D3 that converts T4 into reverse T3 (rT3) or also referred to as the ‘Hibernation hormone…What is this rT3?. When the body is experiencing dysfunction caused by the conditions outlined above including an inflammatory response ( which may be long term), chronic illness, autoimmune Dysfunction and STRESS, to conserve energy, T4 is converted into the inert form of T3, called reverse T3(rT3), an intelligent response of the body. When this happens it is generally due to reduced transport of T3/T4 into the cell as opposed to increased T4 to T3 conversion and thus a marker for reduced cellular uptake of T3 and T4 which cannot be identified with the normal TSH or serum T4/T3 Tests. Suffice to say healthy rT3 and T3 ratios are maintained by good nutrition without starvation signalling. As you can see from the diagram below Cortisol the anti-inflammatory stress hormone released from the adrenals in response to host stress, inhibits TSH and the conversion of T4-T3 causing the thyroid to convert more reverse T3 (rT3) from T4.
How can we fix the problem
- Since the liver is primarily responsible for T4-T3 conversion we need to ensure the liver functions efficiently so detoxing the liver would be a good idea
- Improve diet which might mean a complete dietary and lifestyle change to ensure good nutrition. That means plenty of fruit and vegetables including the green leafy variety like swiss chard, beet greens, kale etc. Juice or blend is a great idea and plenty of sulphur rich food such as cauliflower, onions,garlic, eggs
- Supplementation with whole food supplements that contain specifically Selenium ( for the thyroid deiodinase enzymes), folate ( green leafy veg) and methionine ( red meat) for efficient methylation, all the essential amino acids including Cysteine, Glycine and Glutamate for glutathione production
- Keep stress under control..daily exercise even walking for half an hour a day is beneficial and plenty of rest and sleep
- Ensure good gut health, limited man made food, plenty of fermented products to reseed beneficial flora and yoghurt to feed your beneficial flora and maintain a clean colon ( no need for any dangerous procedures like colonoscopies).
Conclusions

“So Watson, I am sure you will agree that thyroid dysfunction is not just about the thyroid it is invariably the environment around it which is potentially causing the problem”
“ Utterly agree dear boy..that’s why you are the detective of choice from Baker street”.
“ Ok Watson..no time to dilly dally..there is work to be done..time to fix the thyroid “
References/Acknowledgments :
- Triiodothyronine, Interferon Gamma, TBX21, HPT Axis wikipedia
- Imbalance in T cell related transcription factors among patients with Hashimoto’s Thyroiditis Safdari, Alijani, Nemati, Jafarzadeh NCBI 2107
- Hashimotos & Graves disease: The X Factor in thyroid diagnosis & treatment Martin Rutherford, Randall Gates 2017 healthy beginnings
- Hyperthyroidism symptoms Milas,Suri/ Hypothyroidism symptoms James Newman Endocrine Web
- Levothyroxine sodium Mediaonenet.com
- T Bet in disease Nature Immunology
- Thyroid solutions: Glutathione & the T4,T3 Conversion Michael Mcevoy 2015 Metabolic Healing
- Deiodinases: implications of the local controls of thyroid hormone action Bianco Kim 2006 NCBI
- 5 keys to improving thyroid hormone conversion Marc Ryan Hashimoto’s healing library
- Understanding reverse T3 Mary Shaman 2018 Very well health
- Thyroid hormone transport into cellular tissue Kent Holtorf 2014 Association for the advancement of restorative medicine (AARM)
- Functional medicine approach to healing hypothyroidism & Hashimotos Angela Pifer 2014
- Clearing up confusion about reverse T3 Margaret Groves 2015 ZRT Laboratory
- Role of the Iodothyronine Deiodinases in the physiology and pathology of thyroid hormone action Lauren & Zanacki 2013 NCBI
- Hidden causes # 14: Why you still have low thyroid symptoms – Leaky Gut causing low T3 David Clark 2013 Triangle low thyroid solutions
- Discovery of the microbiome Kara Rogers Encyclopedia Britannica
- Common lab values Global RxPH
- Oxidative stress & antioxidant status in Hypo-Hyperthyroidism Patrulea, Muresan, Duncea Researchgate 2012
My name is Eric Malouin
In terms of my heritage I am not a thoroughbred, I am half English from England and half French Canadian from Quebec. Having spent the last 10 years in Medical research I thought that it was time to share my passion for true health to anybody interested in maintaining health without using conventional medicine. Once in the distant past I lived off conventional grocery shelves until you visit the man in the white coat and then a light shines through the darkness that you had not realized you were in… I was in..the twilight zone….I cured my own problems using natural methods, although they were not a big deal since I have always exercised..jogging every morning and tennis 12 hours/week, swimming but I was eating a lot of devil food that was causing my body to become unbalanced..an easy fix..reprogrammed my taste buds and gave the food back to the devil…lol
I hope you enjoy the articles……